Angle-Closure Glaucoma
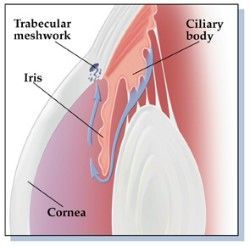
In a normal eye, the fluid in the front part of the eye, the aqueous humor, is produced and exits the eye exerting just enough pressure to keep the eye properly formed without damaging it. That is, the amount of new aqueous that is constantly being created by the eye is balanced by the amount that is constantly draining out of the eye at a place in the eye called the “angle.” (Figure 3) The angle received its name as the angle where the iris meets the cornea.
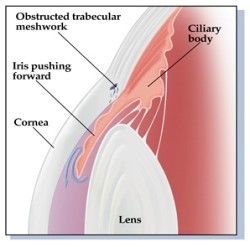
An angle of 15 degrees between the iris and cornea means a much smaller anterior chamber of the eye with little space between the iris and Schlemm’s Canal, the actual drain of the eye, than would be seen with a 30 degree angle. If the angle gets blocked, fluid will continue to be made at a normal rate but will be unable to exit the eye, allowing the pressure in the eye to build up to a harmful level. This is what happens in one type of glaucoma known as “angle-closure” glaucom.
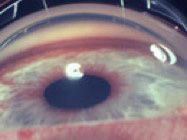
Figure 3 The angle of the anterior chamber of the eye, i.e., the junction of the cornea and sclera externally and the iris internally. The drain of the eye, the canal of Schlemm, is covered by a sieve of tissue called the trabecular meshwork. In this picture it is the thin circular brown line in front of the iris. The brown pigment has been sieved out of the fluid in the anterior chamber (aqueous humor) and deposited in the trabecular meshwork.

The angle may not be allowing sufficient outflow for a variety of reasons. If the person was born with a narrow angle, it will become even narrower with age. If the angle becomes too narrow, the iris may become caught in the drain, blocking it.
Or it may be not be draining properly because a blow to the eye loosened the lens, allowing it to move forward and push the angle closed.
Another possibility is that diabetes has caused abnormal blood vessels to grow over the angle, stimulating scar formation in such a way that the iris has been pulled onto the surface of the angle, again blocking the outflow of aqueous. These three types of angle-closure are just a sampling of the problems that can keep the eye’s drain from working properly. You might suspect, and you would be right, that these very different causes of blockage call for very different types of treatment.
For example, a person born with a narrow angle that has become even narrower with age can be treated by using a laser to make a tiny hole in the iris, allowing the aqueous to drain out more easily. This procedure, known as laser iridotomy (that is, making a tiny hole in the iris with a laser), is useful in cases in which the iris has come forward to block the drain. The hole allows the pressure in front of and behind the iris to be equalized, so that it falls back towards its proper position. With the iris away from the outflow drain, the aqueous humor is again allowed to pass out of the eye normally. Laser iridotomy is extremely effective in many cases of angle-closure glaucoma, but it is important that it be done before the angle closes off. Thus, patients need examinations of the anterior chamber angle to determine if they are predisposed to this problem.
The person with an angle-closure glaucoma caused by a dislocated lens, the second example given, probably should have the dislocated lens removed, so that the angle opens back up naturally. This can be a hazardous procedure and should be done only after careful consideration. However, if it is done at the appropriate time, the pressure will return to normal, and no more damage will occur.
A totally different kind of treatment is required for an angle blocked by abnormal blood vessels, the third type of “angle-closure” mentioned above. It is extremely difficult to make a drain full of abnormal blood vessels work again. Thus, when people are predisposed to getting this type of glaucoma, it is important to take all possible preventive steps addressing the basic causes of these abnormal vessels. Such causes include blockage of the artery or vein that supplies and drains the retina, tumors in the eye, diabetic vessel changes, or inadequate blood flow to the eye (as happens when the large arteries in the neck are blocked).
If the development of abnormal new blood vessels is caught early enough, when the abnormal vessels are just beginning to form, laser treatment of the retina can often be helpful. But once the angle is closed with blood vessels, the angle drainage mechanism is usually permanently damaged, so some type of surgery is usually required to bring the pressure back to a safe level. This may involve placing a plastic drain (an aqueous shunt) that bypasses the blocked angle and allows the aqueous to exit the eye to be absorbed into the vessels outside the eye.
You can begin to see that, even though a diagnosis of “angle-closure glaucoma” is more helpful than a diagnosis simply of “glaucoma,” appropriate treatment requires a specific understanding of just what is causing the pressure in the eye to be at harmful levels.
But even knowing the specific reason for angle-closure is still not enough. The doctor also must judge when and to what extent the patient, because of deteriorating vision, will begin to have difficulty doing things he’s used to doing.
At the low end of the scale, it may be that the cause of damaging high pressure may have disappeared, so that no more damage will occur. If this is the case, the best treatment is often no treatment.
Another possibility is that the glaucoma is progressing slowly, so slowly that the eye probably will lose only a little bit of vision even over a period as long as 25 years. In such cases, although some treatment is necessary to lower the pressure, the treatment should carry with it as little risk of harmful side effects as possible.
On the other hand, in some cases, when, for example, the angle suddenly becomes completely covered by the iris, glaucoma damage may occur very rapidly, leading to total blindness within a few hours. Even here, however, each case is different. In some cases, when the pressure is very high, the tissue that produces the fluid (the ciliary body) may stop making fluid so that the pressure doesn’t stay high for long. In these cases, the pain may be very severe, but vision will be impaired only temporarily.
The most common form of angle-closure glaucoma is relative pupillary block. In relative pupillary block, aqueous pressure behind the iris plane forces the iris anteriorly. Elimination of this pressure gradient can be achieved with laser iridotomy. A second, less common form of angle-closure glaucoma is known as plateau iris syndrome. In plateau iris, the iris is forced into the angle by the presence of an abnormally placed, anterior ciliary body. Because this form of angle-closure is not due to fluid pressure gradient, it responds poorly to laser iridotomy. If undiagnosed, recurrent angle-closure may develop. Other forms of angle-closure of interest to clinicians include lens-induced angle-closure, iris cysts, iris tumors, ciliary body rotation due to effusion, dark room provocative testing during ultrasound biomicroscopy, malignant glaucoma.
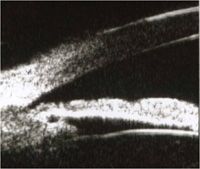
Relative pupillary block is the most common form of angle-closure glaucoma. Resistance to aqueous movement from its site of production by the ciliary epithelium within the posterior chamber through the pupil produces a pressure gradient across the iris which forces the iris anteriorly, into the trabecular meshwork, thereby closing the angle. This give the iris its typical convex configuration on ultrasound biomicroscopy (top).

The most important anatomic landmark, particularly in the evaluation of the angle-closure glaucomas is the scleral spur, which can be seen an the innermost point of the line separating the ciliary body and the sclera. The trabecular meshwork is located directly anterior to this structure. If aqueous humor, which has no reflectivity and is therefore black on ultrasound biomicroscopy, has access to the meshwork, the angle is open.
Following laser iridotomy, aqueous has free access to the anterior chamber and the pressure gradient is eliminated. The iris assumes a flat (planar) configuration and the angle opens (bottom).
The reasons why some individuals with narrow angles develop angle- closure while others do not is not clearly understood. One factor which can affect angle configuration is the amount of illumination, which alters pupillary size. Under normal conditions, the miotic response to light causes the angle to open (top).
If the room illumination is dimmed during scanning of the patient shown above, pupillary dilation may cause the peripheral iris to crowd the and become apposed to the trabecular meshwork, causing angle closure (bottom).
Not all angle-closure is caused by relative pupillary block. In plateau iris syndrome, the physical presence of an anteriorly placed ciliary body forces the peripheral iris into the angle. Iridotomy relieves the contribution of pupillary block component to the angle narrowing, but not the closure related to the abnormal ciliary body position. Laser iridoplasty is often useful under these circumstances.
A large, intumescent lens or forward lens movement due to zonular laxity or dehiscence may cause mechanical crowding of the angle.
Focal forms of angle-closure may be induced by cystic or solid masses involving the iris or the ciliary body. Iridociliary cysts are characterized by an echolucent interior.
Tumors or infiltration of the iris or ciliary body may also cause angle-closure and are characterized by uneven internal echoes when compared to cystic structures.
Malignant glaucoma, an infrequent cause of postoperative angle-closure glaucoma, can result from aqueous misdirection or from annular ciliary body detachment. In either case, anterior rotation of the ciliary body about its insertion into scleral spur may cause a secondary angle- closure glaucoma.

Contact Us
We will get back to you as soon as possible.
Please try again later.

Manhattan Office

Queens Office

Navigation