Retinopathy
Diabetic Retinopathy
Diabetic retinopathy usually occurs in patients who have had diabetes for several years. There is damage that occurs to the lining of the blood vessels inside the retinal tissue of the eye. Early on, patients with diabetic retinopathy do not notice decreased vision.

Therefore, it is vitally important that once you are diagnosed with diabetes, you undergo a dilated retinal exam once a year. You must take control of your diabetes by eating a healthy diet, exercising, following your medical doctor’s treatment plan, keeping your sugar under control and following up with your eye doctor on a regular basis.
Early symptoms of blurred vision are the most common. This occurs when the glucose level is very high, thereby altering the natural state of the lens in the eye. The blurred vision improves once the sugar level is under control.
Types of Antiglaucoma Drugs:
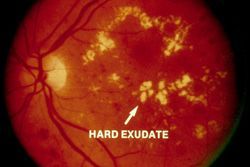
- Early diabetic retinopathy. Nonproliferative diabetic retinopathy (NPDR) is the most common type of diabetic retinopathy. It can be described as mild, moderate or severe. When you have NPDR, the walls of the blood vessels in your retina weaken. Tiny bulges protrude from the vessel walls, sometimes leaking fluid and blood into the retina. These bulges are called microaneurysms. Nerve fibers in the retina may begin to swell. Sometimes the central part of the retina (macula) begins to swell, too. This is known as macular edema.
- Advanced diabetic retinopathy. Proliferative diabetic retinopathy (PDR) is the most severe type of diabetic retinopathy. When you have PDR, abnormal blood vessels grow in the retina. Sometimes new blood vessels grow or leak into the clear substance that fills the center of your eye (vitreous). Eventually, scar tissue stimulated by the growth of new blood vessels can lead to a retinal detachment. If the new blood vessels create scarring in the drainage angle of the eye, pressure may build up and cause glaucoma. This can damage the nerve that carries images from your eye to your brain (optic nerve).

The longer you have diabetes, the greater your risk of developing diabetic retinopathy.
Uncontrolled diabetes and diabetic retinopathy can lead to complications such as:
- Vitreous hemorrhage. The new blood vessels may bleed into the vitreous. The blood may appear as black spots to you or completely block your vision. Vitreous hemorrhage by itself usually doesn’t cause permanent vision loss. The blood often clears from the eye within a few weeks. We usually ask patients to sleep in a sitting position to allow the blood to settle out of the visual axis. If, after one month the blood does not clear, we then consider surgical removal of the blood with vitrectomy.
- Retinal detachment. Scar tissue can pull the retina away from the back of the eye. This may cause spots floating in your vision, flashes of light or severe vision loss and blindness. This is a surgical emergency that should be addressed within several hours.
- Neovascular Glaucoma. New blood vessels may grow in the front part of your eye and block off the trabecular meshwork (drain in the front of the eye), leading to glaucoma.
Preparing for Your Appointment
- Write down a brief summary of your diabetes history, including who your doctors are, a list of your medications and a summary of your symptoms.
Tests and Diagnosis
We will take your medical and surgical history and obtain information on all of your medications and allergies. We will check your vision, ocular motility, papillary examination, intraocular pressure, examine the drainage angle, check for cataracts and perform a dilated retinal exam. If retinopathy is detected, you may also have a retinal photography test called fluorescein angiography. First, we will dilate your pupils and take pictures of the inside of your eyes. Then you will receive an injection of a special dye into your arm. More pictures will be taken as the dye circulates through your eyes. We will then show you the images of blood vessels that are closed, broken down or leaking fluid.
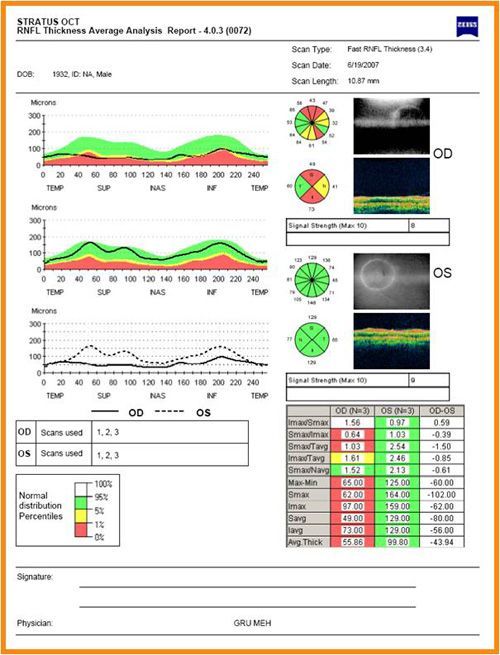
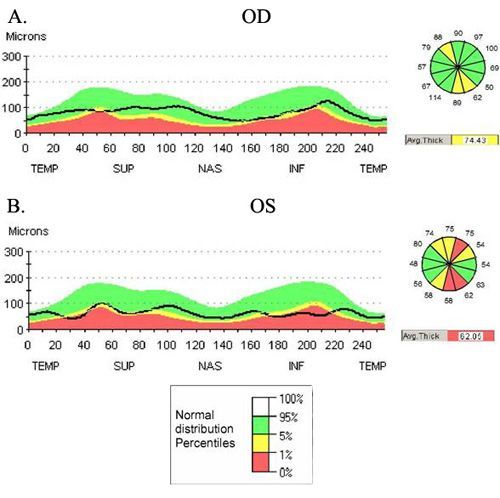
Optical Coherence Tomography
We may also perform an optical coherence tomography (OCT) exam. This imaging test provides cross-sectional images of the retina that show the thickness of the retina, which will help determine whether fluid has leaked into retinal tissue. Later, OCT exams can be used to monitor how treatment is working.
Treatments for Diabetic Retinopathy
Early diabetic retinopathy
If you have early nonproliferative diabetic retinopathy, you may not need treatment right away. However, you will need to be closely monitored and maintain good blood sugar control. When diabetic retinopathy is in the mild or moderate stage, good blood sugar control can slow the progression of diabetic retinopathy.
Advanced diabetic retinopathy
If you have proliferative diabetic retinopathy, you’ll need prompt surgical treatment which may include:
- Focal laser treatment. This laser treatment, also known as photocoagulation, can stop or slow the leakage of blood and fluid in the eye. This is performed in our office. During the procedure, leaks from abnormal blood vessels are treated with laser burns. Focal laser treatment is usually done in a single session. Your vision will be blurry for about a day after the procedure. Sometimes you will be aware of small spots in your visual field that are related to the laser treatment. These usually disappear within weeks. If you had blurred vision from swelling of the central macula before surgery, however, you may not recover completely normal vision.
- Scatter laser treatment. This laser treatment, also known as panretinal photocoagulation, can shrink the abnormal blood vessels. This is also performed in our office. During the procedure, the areas of the retina away from the macula are treated with scattered laser burns. The burns cause the abnormal new blood vessels to shrink and scar. Your vision will be blurry for about a day after the procedure. Some loss of peripheral vision or night vision after the procedure is possible.
- Vitrectomy. This procedure can be used to remove blood from the middle of the eye (vitreous) as well as any scar tissue that’s tugging on the retina. It’s done in a surgery center or hospital under local or general anesthesia. Scar tissue and blood in the eye are removed with delicate instruments and replaced with a salt solution, which helps maintain your eye’s normal shape. Sometimes a gas bubble must be placed in the cavity of the eye to help reattach the retina. If a gas bubble was placed in your eye, you may need to remain in a facedown position until the gas bubble dissipates — often several days. You’ll need to wear an eye patch and use medicated eye drops for a few days or weeks. Vitrectomy may be followed or accompanied by laser treatment.
Surgery often slows or stops the progression of diabetic retinopathy, but it’s not a cure. Because diabetes is a lifelong condition, future retinal damage and vision loss is possible. Even after treatment for diabetic retinopathy, you’ll need regular eye exams. At some point, additional treatment may be recommended.
Prevention
If you have diabetes, reduce your risk of getting diabetic retinopathy by doing the following:
- Make a commitment to managing your diabetes. Make healthy eating and physical activity part of your daily routine. Take oral diabetes medications or insulin as directed.
- Monitor your blood sugar level. You may need to check and record your blood sugar level several times a day — more frequent measurements may be required if you’re ill or under stress. Careful monitoring is the only way to make sure that your blood sugar level remains within your target range. Ask your doctor how often you need to test your blood sugar.
- Ask your medical doctor about a glycosylated hemoglobin test. The glycosylated hemoglobin test or hemoglobin A1C test reflects your average blood sugar level for the two- to three-month period before the test. For most people, the A1C goal is to be under 7 percent. Remember, keeping your blood sugar level as close to normal as possible slows the progression of diabetic retinopathy and reduces the need for surgery.
- Keep your blood pressure and cholesterol under control. High blood pressure and high cholesterol increase the risk of vision loss. Eating healthy foods, exercising regularly and losing excess weight can help. Sometimes medication is needed, too.
- If you smoke or use other types of tobacco, ask your doctor to help you quit. Smoking increases your risk of various diabetes complications, including diabetic retinopathy. Talk to your doctor about ways to stop smoking or using other types of tobacco.
- Pay attention to vision changes. Yearly dilated eye exams are an important part of your diabetes treatment plan. Contact your eye doctor right away if you experience sudden vision changes or if your vision becomes blurry, spotty or hazy.
Remember, diabetes doesn’t necessarily lead to poor vision. Taking an active role in diabetes management can go a long way toward preventing complications.

Contact Us





